 When it rains, it pours. I’m currently taking care of 5 patients who have blood infections from Staphylococcus aureus (commonly referred to as staph).
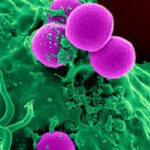
When it rains, it pours. I’m currently taking care of 5 patients who have blood infections from Staphylococcus aureus (commonly referred to as staph).
Staph is a topic I did several posts about, in the earlier days of the blog. It remains a very relevant topic, being one of the commonest infectious diseases I get called about in the hospital. Some cases of staph infection are uncomplicated and pretty straight forward. Others are very complexed, causing quite a bit of stress for the patient and their family, as well as for the doctors caring for the patient.
Related post: That stick staph!
My current cases of complicated staph infection all have the staph in their blood, and are as follows:
Patient 1 – Forty something year old who lives in a nursing home due to inability to care for self, has no major medical problems except for mental illness. Confusion developed suddenly one day so the nursing home sent the patient to the hospital for evaluation. Cultures were done as part of this evaluation, and staph was found to be growing in the blood. In this case, there was no obvious source (such as a skin infection) of the staph.
Patient 2 – Fifty something year old on dialysis for the past ~5 years, via a fistula (a surgically created vein used to remove and return blood during hemodialysis) in the arm, had an ulcer on the ankle for almost a year. This formed due to complications from diabetes, including poor circulation and neuropathy (no feeling in the feet). The ulcer suddenly got worst causing fever, prompting a visit to the doctor who referred the patient to the hospital. The surgeon took the patient to the operating room and found a large amount of pus in the ankle joint. The culture was positive for staph. The patient’s blood cultures subsequently came back positive for…you guessed it…staph!
Patient 3 – Sixty something year old with lots of problems (diabetes, hypertension, kidney failure) has been living in a nursing home due to a stroke. The patient has been on dialysis for the past year, via a catheter in the chest (compared to the fistula in patient #2) and was sent from the nursing home due to fever and worsening confusion. Blood cultures came back positive for staph.
Patient 4 – Fifty something year old with issues related to chronic pain and depression, has been in and out of hospital over the years for various complaints. This patient had a mediport (a device placed under the skin, usually in the chest, for administration of medication, and for drawing of blood samples) placed 5 years ago. The family noticed persisting confusion and decided a visit to the ER was necessary. Infection was sought as one of the possible causes of confusion, and the blood cultures came back positive for staph. It turned out that the mediport was infected, to the point where there was an infectious mass (a vegetation) at the tip of the tubing from the port. The mass sat on the wall of a large blood vessel leading to the heart.
Patient 5 – Forty something year old with long standing severely uncontrolled diabetes, whose blood is so ‘sweet’ that the skin constantly itches, and has a ‘bumpy’ rash all over. For the second time in less than a year, all this itching caused a sore that got infected with staph. The sore once again turned into a large abscess. Only this time, the abscess was so extensive that the staph escaped from it, and into the blood stream, causing the patient to get very ill with fever and weakness. This is what prompted the hospital emergency room visit.
Related post: MRSA – 3 things that make this little bug a big deal
There are many different species of staph, but of the few most harmful species, Staphylococcus aureus is, by far, one of the most dangerous. This species of staph may, or may not, be sensitive to the killing effect of penicillin type antibiotics (methicillin sensitive Staphylococcus aureus – MSSA, versus methicillin resistant Staphylococcus aureus – MRSA).
Many patients get quite fearful at the thought that they may have an infection with MRSA as opposed to MSSA. The fact is, however, that both types of staph can cause the same complicated, disabling infections. The advantage with MSSA however, is that the antibiotics used to treat it, are less harsh (and often less expensive) than those used to treat MRSA.
“The advantage of MSSA over MRSA is that less harsh (and expensive) antibiotics are required to treat it.”
Of the 5 patients listed above, only one had infection with MRSA. The other 4 had MSSA.
Staphylococcus aureus in the blood is always a massive deal. It should never be taken lightly, and should always be treated with intravenous antibiotics. Treatment is usually for at least 4 weeks on average, but longer or shorter, depending on the individual clinical situation.
Complications in patients with staph blood stream infections, may arise months later, if their treatment was for too short a period, or if it was with oral antibiotics instead of intravenous antibiotics.
All the patients above had scans (echocardiograms) of their hearts to evaluate whether or not the infection had affected their heart valves (a common complication of staph blood stream infection). Only patient 4 had a scan showing infection in a large vessel leading to the heart.
The good news is, that most staph infections are simple skin infections, and don’t even require a visit to the doctor’s office, much less a hospital admission. In the event that medical treatment is needed for staph, most persons will recover uneventfully.
Related post: 8 strategies to prevent MRSA infection
Then persons who have the most complicated course after a staph infection, are those who have multiple medical problems (as you probably noticed in the examples), requiring them to be in and out of hospital frequently. Patients who have artificial devices in their bodies (such as dialysis catheters, pacemakers, artificial joints, etc) are also prone to complicated staph infections.
Regular doctors can definitely treat complicated staph infections. However, having an infectious diseases specialist on the case, can sometimes help with streamlining of the management plan.
 Lajune says
Lajune says
October 16, 2016 at 2:59 pmVery interesting
 infectiousmd says
infectiousmd says
October 17, 2016 at 11:33 amThank you for supporting the blog!