 I’ve been meaning to write about staph for a long time as it is one of the commonest infectious diseases I treat. In this post I will give you an idea what staph is, how it gets into the body, how it ends up causing serious infections, and why some people get nightmarish complications and others not.
I’ve been meaning to write about staph for a long time as it is one of the commonest infectious diseases I treat. In this post I will give you an idea what staph is, how it gets into the body, how it ends up causing serious infections, and why some people get nightmarish complications and others not.
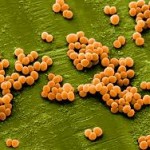
‘Staph’ infections are some of the commonest I see on a daily basis. ‘Staph’ is short for Staphylococcus which is a bacterium (type of germ) found on our skin, in our nostrils, and in the environment in general, particularly on surfaces which are touched frequently. There are many different species or types of staph, some not as harmful as others. One of the most important types of staph is Staphylococcus aureus. This is the type of staph most likely to cause infection serious enough to result in admission to hospital. In this post, when I refer to staph, I am talking about Staphylococcus aureus.
I like to describe the germ Staphylococcus aureus as having ‘protean clinical manifestations’ meaning that it can cause just about any type of infection in the body (ID trivia – other germs with protean clinical manifestations include tuberculosis and syphilis). The problem with staph is that it is very sticky – meaning that it can easily lodge into structures of the body like muscles, joints – especially those that have been replaced, the spine, heart valves, the prostate gland… anywhere, really.
How does staph get to these faraway places of the body anyway?
An obvious way is if it is introduced directly by a medical procedure such as a knee injection for arthritis, a back injection for chronic pain, a prostate biopsy, after any surgical operation. Another common way is via a chronic wound, such as a diabetic foot ulcer with infection spreading from the ulcer to the underlying bone. Many patients with bad staph infections never had any of these procedures and in those cases what probably happened is that there was a staph skin infection as minor as a pimple, or more serious such as an abscess. The bacteria then escaped from the skin infection into the blood stream. It then circulated in the blood and got lodged in one of the areas mentioned above. There are many cases where it is not obvious where the staph came from. In those instances, an insignificant scratch or cracked area of skin could have been the entry point for the staph.
What determines where staph eventually lodges?
It is usually an area with some loss of integrity, or defect, where staph chooses to set up its new home. Areas damaged by arthritis such as the spine or a joint are common. Damaged heart valves are also prone to having staph get stuck to them. A big problem nowadays is foreign material in the body. There are many ways in which our bodies can be “patched up” such as with joint replacements, rods and screws for broken bones, pacemakers for heart problems, artificial heart valves, implanted pumps, etc. The problem with these devices is that they do not have blood vessels penetrating them and supplying blood. A blood supply is necessary to wash away toxins/germs and promote healing. Because there is no blood supply, germs like staph can stick onto these foreign devices. Staph then protects itself by forming a protective film around it so that the immune system’s fighter cells and even antibiotics cannot get to it.
What happens after staph sticks somewhere in the body?
After lodging into one of the deep, dark areas of the body the staph hides out and multiplies, or as I like to say, ‘brews’ over time. As it multiplies, the body sends fighter white blood cells (pus cells) to the area and eventually there is a lot of swelling and inflammation and an abscess may form. If the affected area is a joint, the bacteria and fighter white cells increase in the joint fluid and it starts to look like pus! By now of course, the joint is very painful and often swollen.
Why do some people get nightmare complications from staph and others don’t?
Most people who have staph on their bodies – on the skin or in the nostrils – will never actually get an infection. It remains dormant, hanging out in balance with all the other ‘commensal’ germs (remember, our bodies are not sterile, there are germs everywhere!). If staph does get introduced into the blood stream, it doesn’t always cause major problems. As long as the immune system is in tip top shape, it gets to work briskly and eradicates the staph before it gets a chance to ‘stick’ somewhere. However, if for some reason the immune system is not able to overcome the infection, then things can start to go wrong, with one of more of the above mentioned manifestations occurring.
Staph is a really large topic and there are many things I have not said about it in this short post. What I tried to do is give you an idea of what sort of germ staph is, the type of havoc it can wreak on the body and who is more likely to get complicated staph infections.
In my next blog post, I will go into more detail about some of the complications of staph infection. I will also delve into the difference between sensitive and resistant Staphylococcus aureus – MSSA vs MRSA. Don’t forget to check back to learn more!
 Dean says
Dean says
April 24, 2019 at 5:54 pmI have recently read of a form of treatment resistant Candida Aureus that could become more of a problem in the U.S. Do you have any information about that as to prevention and signs of the infection for a layperson?
 infectiousmd says
infectiousmd says
May 29, 2019 at 2:37 pmHi Dean,
Thank you for your question and sorry for the delayed response.
Serious infections with Candida auris are a problem mainly for persons who already have serious medical issues resulting in them needing to have ports and intravenous lines for prolonged periods of time.
Examples would be persons undergoing chemotherapy for cancer, or persons who are not able to eat and therefore need nutrition via an intravenous line which would be left in place for many months at a time. Another set of persons at risk would be those who require antibiotics for long periods of time as they can have a depletion of the normal bacteria in their body, and therefore be at increased risk for yeast infections including those with C. auris.
For the vast majority of us, C. auris will never be a problem. It is not something that is contagious, therefore we don’t have to worry about catching it.
C. auris can be curable, but the problem with deaths from it has to do with the fact that the infected/affected persons are already very sick and so are at higher risk of dying from any infection, not only C. auris.
Bottom line, these infections are uncommon, and as long as we maintain optimum health as much as possible, we are not likely to ever have to battle this infection.
If you think you may be at risk for any infection, definitely schedule an appointment with your personal doctor for further evaluation.
Thank you for reading and be healthy!
AG